Addiction is a chronic condition with a mix of contributing factors. Genetics play a significant role, with family history increasing a person’s vulnerability. Mental health conditions like depression or anxiety can also make someone more susceptible to seeking relief through addictive behaviors.
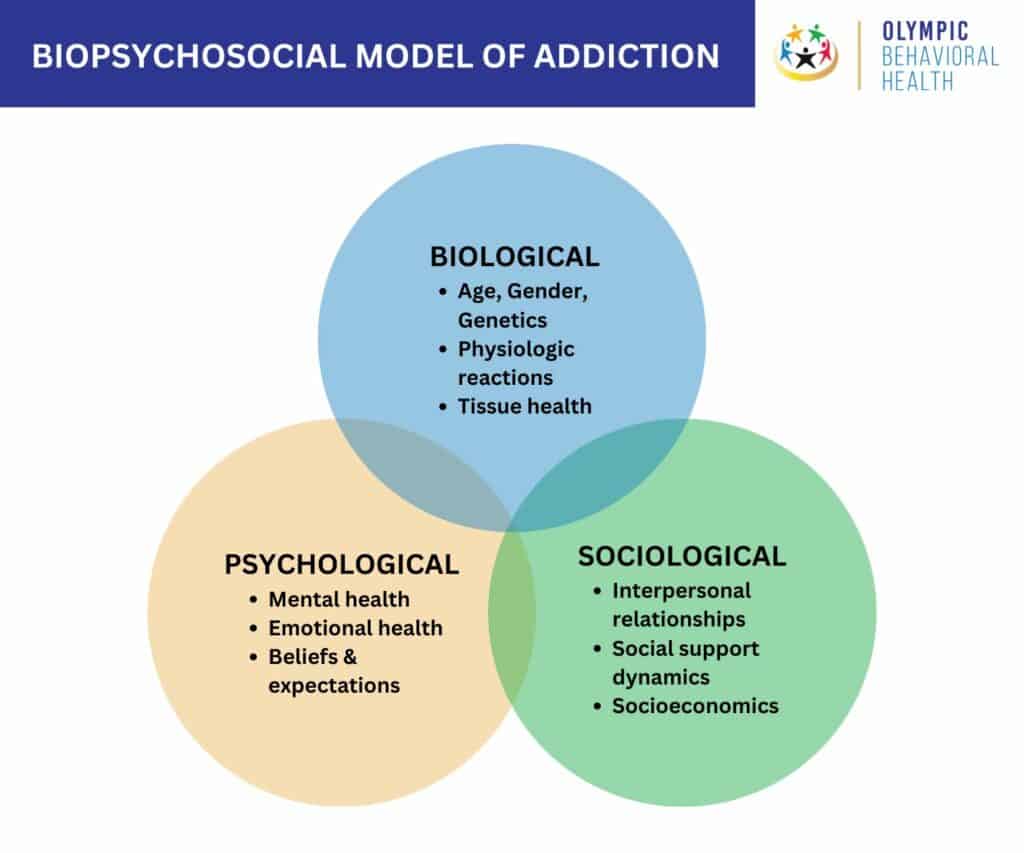
The biopsychosocial model emphasizes the interaction of biological, psychological, and social factors. Biology includes genetics and brain chemistry, while psychology examines an individual’s thoughts, emotions, and coping mechanisms. Social factors include influences like family, friends, and socioeconomic status.
Personality theories suggest certain personality traits, like impulsivity or risk-taking, can make someone more prone to addiction. These traits might lead them to experiment with addictive substances or behaviors more readily.
Neuropsychology focuses on the brain’s role in addiction. Addictive substances and activities hijack the brain’s reward system, leading to cravings and withdrawal symptoms. Over time, the brain adapts to the presence of the addictive substance, making it harder to experience pleasure without it.
What is the Biopsychosocial Model of Addiction?
The biopsychosocial model of addiction is a holistic approach that views addiction as arising from a complex interplay of biological, psychological, and social factors. This means that there isn’t just one cause of addiction but rather a combination of influences that can make someone more or less likely to develop an addiction.
The biopsychosocial model of addiction is credited to American psychiatrist George Engel. He proposed this model in 1977 as a more comprehensive way to understand illness, including mental health disorders, rather than solely focusing on biological factors.
Components of the biopsychosocial model of addiction include:
- Biological factors include genetics, brain chemistry, and overall physical health. For example, people with a family history of addiction are more likely to develop an addiction themselves. This is because they may have inherited genes that make them more susceptible to the rewarding effects of drugs or alcohol. Brain chemistry also plays a role. Addictive substances can alter the brain’s reward system, making it difficult to resist cravings and continue using the substance.
- Psychological factors include mental health conditions, personality traits, and coping mechanisms. For example, people with depression or anxiety are more likely to develop an addiction. This is because they may use drugs or alcohol to self-medicate their symptoms. Personality traits such as impulsivity and sensation-seeking can also increase the risk of addiction.
- Social factors include social norms, peer pressure, and access to drugs or alcohol. For example, people who live in environments where drug or alcohol use is every day are more likely to develop an addiction themselves. Peer pressure can also play a role, as can easy access to addictive substances.
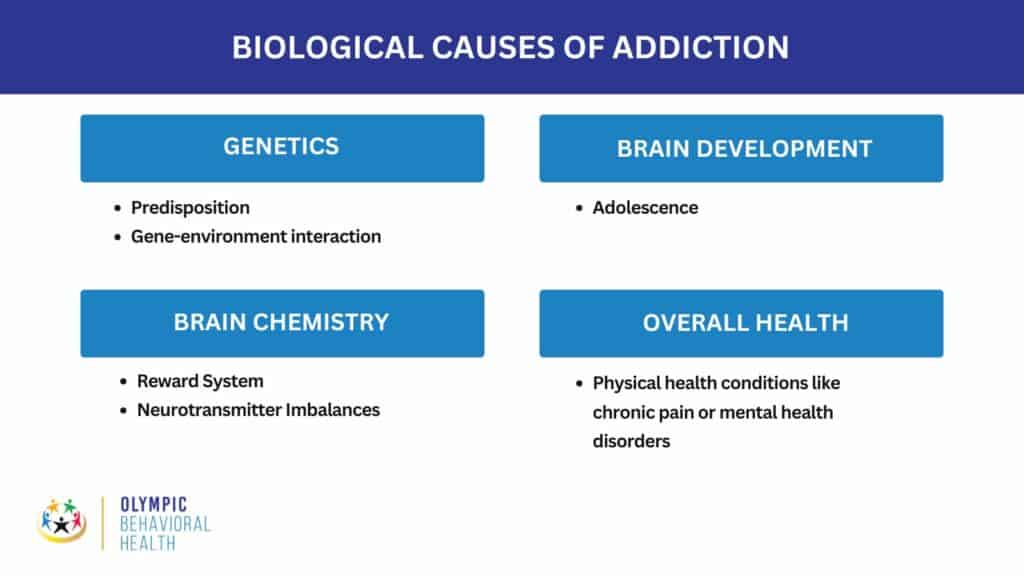
What are the Biological Causes of Addiction?
Biological factors that increase an individual’s risk of developing an addiction include their genetic makeup, brain chemistry, brain development, and health status. Here’s a breakdown of some key biological influences.
Genetics
- Predisposition: Genes can influence how your body processes substances, making you more or less likely to experience the pleasurable effects or become dependent. Addiction tends to run in families, but it’s not a simple inheritance pattern.
- Gene-environment interaction: Genes don’t guarantee addiction. Environmental factors like childhood trauma can influence how genes are expressed, potentially increasing addiction risk.
Brain Chemistry
- Reward System: Addictive substances hijack the brain’s reward system, usually activated by pleasurable experiences like eating or socializing. Drugs or alcohol cause a surge of dopamine, a neurotransmitter associated with pleasure and reward. This reinforces the desire to repeat the experience and can lead to compulsive drug-seeking behavior.
- Neurotransmitter Imbalances: Chronic substance use can disrupt the balance of neurotransmitters in the brain, affecting mood, motivation, and self-control. This can make it difficult to experience pleasure from everyday activities and intensify cravings for the substance.
Brain Development
- Adolescence: The brain’s reward system continues to develop throughout adolescence, making teens more susceptible to the rewarding effects of drugs and alcohol. Early use of substances can also negatively impact brain development, further increasing addiction risk.
Overall Health
- Physical health conditions like chronic pain or mental health disorders can create a vulnerability to addiction as people seek relief through substances.
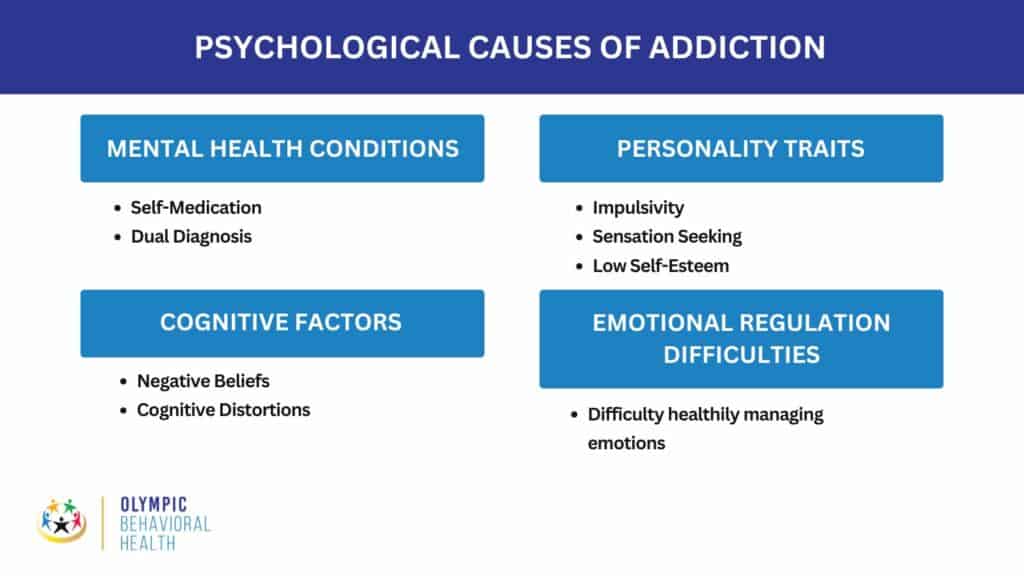
Psychological Causes of Addiction
Psychological factors in addiction development are a significant piece of the puzzle. They encompass a person’s mental health, emotional state, and thought patterns, all of which can influence their vulnerability to addiction and how they use substances. Here’s a closer look at some critical psychological causes of addiction.
Mental Health Conditions
- Self-Medication: People with mental health disorders like depression, anxiety, or PTSD may use drugs or alcohol to try and alleviate their symptoms. This can become a dangerous coping mechanism and lead to addiction.
- Dual Diagnosis: Many people with addictions also have co-occurring mental health disorders. The presence of both conditions can worsen each other, making treatment more complex.
Personality Traits
- Impulsivity: Difficulty controlling impulses can make it harder to resist cravings and continue using substances despite adverse consequences.
- Sensation Seeking: A desire for intense experiences and risk-taking behaviors can lead someone to experiment with drugs or alcohol and potentially develop an addiction.
- Low Self-Esteem: People with low self-esteem may use substances to feel better about themselves, creating a cycle of dependence.
Cognitive Factors
- Negative Beliefs: Unhealthy thought patterns, such as hopelessness or feelings of worthlessness, can make someone more likely to turn to substances for escape.
- Cognitive Distortions: These are unrealistic or negative ways of thinking that can fuel addiction. For example, someone might think, “I can’t cope without this substance,” or “I’m a failure if I quit.”
Emotional Regulation Difficulties
- Difficulty healthily managing emotions can lead to using substances to cope with negative feelings like stress, anger, or sadness.
It’s important to note that these psychological factors don’t cause addiction on their own. However, they can create a vulnerability that, combined with biological and social aspects, can increase the risk of addiction.
Personality Theories in Addiction
Personality theories in addiction explore the connection between personality traits and a person’s vulnerability to addiction. These theories propose that specific personality characteristics can make someone more likely to develop or struggle with addiction. Here’s a breakdown of some key ideas.
Affect Dysregulation Model
This model focuses on how individuals handle emotions, particularly negative emotions. People who have difficulty regulating their emotions, especially negative ones, may be more likely to turn to substances as a coping mechanism.
Subcategories
- Negative Affect: Experiencing frequent negative emotions like anxiety, depression, or anger can increase the desire to use substances to numb these feelings.
- Positive Affect: People who have difficulty experiencing positive emotions may use substances to create feelings of pleasure or excitement.
Impulsivity Models
- These models highlight the role of impulsivity, or the tendency to act without thinking about the consequences, in addiction. People who struggle with impulsivity may have difficulty resisting cravings or engaging in risky behaviors associated with substance use.
- Reward Sensitivity Theory: This theory suggests that people with high reward sensitivity are more likely to seek out intense experiences and sensations, which can lead to substance use and addiction.
Five-Factor Model (FFM)
The Five-Factor Model (FFM), or the OCEAN model, is a widely used theory in personality psychology that identifies five broad personality traits.
These traits are considered the basic dimensions of human personality and can be used to describe a person’s tendencies across different situations.
Here’s a breakdown of the Big Five:
- Openness to Experience (O): This trait reflects intellectual curiosity, imagination, and a preference for novelty and variety. Highly open people are often described as creative, artistic, and eager to learn new things.
- Conscientiousness (C): This trait encompasses organization, self-discipline, goal-oriented behavior, and a strong work ethic. Highly conscientious people are reliable, responsible, and good at planning and following through.
- Extraversion (E): This trait reflects sociability, talkativeness, assertiveness, and a desire for social interaction. People high in extraversion are outgoing, energetic, and enjoy being around others.
- Agreeableness (A): This trait reflects empathy, cooperation, kindness, and a tendency to put the needs of others before your own. People who are high in agreeableness are trusting, helpful, and get along well with others.
- Neuroticism (N): This trait, sometimes referred to as Emotional Stability (its opposite), reflects a tendency to experience negative emotions easily, such as anxiety, fear, sadness, and anger. People high in neuroticism are often moody, worry a lot, and may struggle with stress.
FFM and Addiction
Research suggests that certain traits within the FFM might be linked to a higher risk of addiction:
- High Neuroticism: People prone to negative emotions and anxiety may use substances to cope.
- Low Extraversion: Individuals who are introverted or shy may use substances to feel more social.
- Low Agreeableness: Less agreeable people may be more prone to rebellious behaviors like substance use.
- Low Conscientiousness: Individuals who struggle with self-control and planning may find it harder to resist cravings or stick to treatment plans.
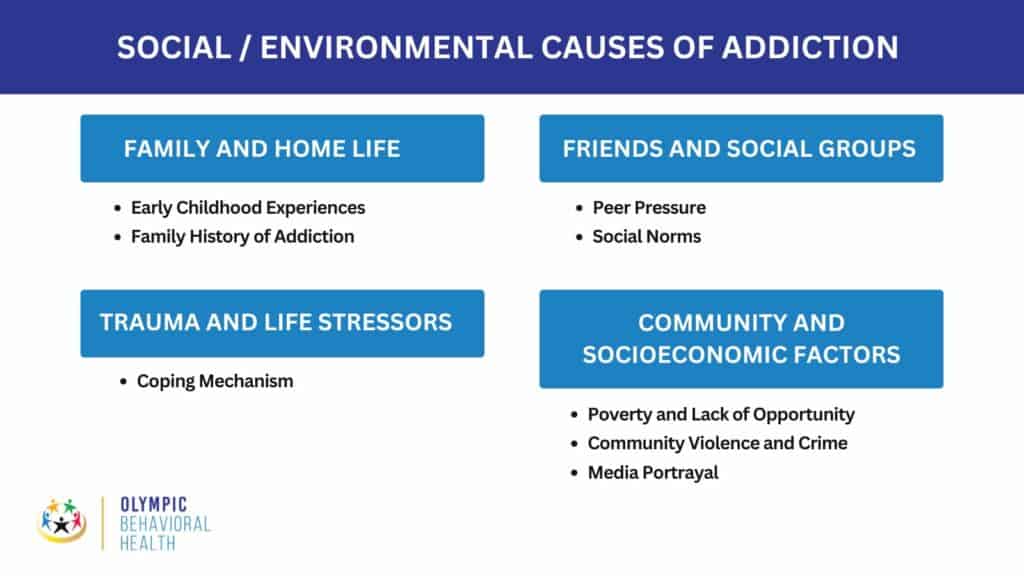
Social / Environmental Causes of Addiction
Social and environmental factors play a significant role in influencing addiction. These factors can create situations that make someone more likely to start using substances, have difficulty quitting, or relapse. Here’s a breakdown of some key social and environmental influences:
Family and Home Life
- Early Childhood Experiences: Traumatic events like abuse, neglect, or witnessing violence can increase addiction risk. Inconsistent parenting styles, either overly permissive or authoritarian, can also make someone more susceptible.
- Family History of Addiction: Having parents or close relatives with addiction increases your risk due to potential genetic predisposition and exposure to addictive behaviors.
Friends and Social Groups
- Peer Pressure: Friends who use drugs or alcohol can pressure you to use as well, especially during adolescence when social acceptance is a strong motivator.
- Social Norms: Cultures with high rates of substance use, or where specific substances are ingrained in social activities, can normalize use and make it harder to resist.
Trauma and Life Stressors
- Coping Mechanism: People may turn to drugs or alcohol as a way to cope with stressful life events, emotional pain, or mental health issues like anxiety or depression.
Community and Socioeconomic Factors
- Poverty and Lack of Opportunity: Limited access to education, employment, and resources can create a sense of hopelessness and fuel substance use as a form of escape.
- Community Violence and Crime: Living in an environment with high crime rates or violence can increase stress and lead to substance use as a coping mechanism.
- Media Portrayal: Constant exposure to glamorized portrayals of substance use in media can make it seem more appealing, especially for young people.
It’s important to remember that social and environmental factors interact with biological vulnerabilities. For instance, someone with a genetic predisposition to addiction may be more likely to develop an addiction if they also experience significant childhood trauma.
Neuropsychology in Addition
Neuropsychology plays a crucial role in understanding and treating addiction. It bridges the gap between the brain and behavior, specifically focusing on how substance use affects brain function and how those changes contribute to addiction. Here’s how neuropsychology is involved in addiction.
Assessment
- Cognitive Deficits: Neuropsychologists can use standardized tests and assessments to identify cognitive deficits caused by substance use. These deficits can affect memory, attention, decision-making, and impulse control, all of which can contribute to addiction.
- Example: A test measuring working memory might reveal difficulty remembering information to complete a task, which can impact the ability to resist cravings or plan for long-term goals.
- Brain Imaging: While not always used in a neuropsychological assessment, neuroimaging techniques like MRI or PET scans can sometimes be used to visualize potential brain abnormalities associated with addiction.
Understanding Addiction Process
Neuropsychology helps us understand how addictive substances alter brain circuits, particularly the reward system and prefrontal cortex. The reward system is responsible for feelings of pleasure and motivation, while the prefrontal cortex is involved in decision-making and impulse control. Chronic drug use can disrupt these systems, leading to intense cravings and difficulty resisting them.
Informing Treatment
- Treatment Tailoring: By identifying specific cognitive weaknesses, doctors can tailor their treatment to address those areas. For example, cognitive behavioral therapy (CBT) can be adapted to improve decision-making skills, while memory training exercises can help with relapse prevention.
- Treatment Monitoring: Neuropsychological assessments can be used to monitor treatment progress. Improvements in cognitive function can indicate successful recovery and a reduced risk of relapse.
Limitations
- The brain is dynamic: The brain is constantly adapting, and some cognitive deficits associated with addiction can improve with abstinence and treatment.
- Not diagnostic: Neuropsychological assessments alone cannot diagnose addiction. They are used in conjunction with other clinical evaluations.
Overall, neuropsychology offers valuable tools for understanding the neurological underpinnings of addiction and creating more effective treatment approaches. By targeting the cognitive and neuropsychological aspects of addiction, treatment can be more comprehensive and lead to better long-term outcomes for individuals struggling with substance use disorders.
Stimulus Control of Behavior in Addiction
Stimulus control of behavior plays a significant role in addiction. It refers to how environmental cues and stimuli can trigger cravings and relapse in individuals struggling with substance use disorders. Here’s a breakdown of this concept and how it relates to addiction, along with some authoritative references for further exploration:
How it Works
- Classical Conditioning: Through classical conditioning, specific environmental cues become associated with the rewarding effects of drugs or alcohol. These cues can be anything from sights and sounds related to drug use (paraphernalia, locations) to emotional states or social situations. Over time, exposure to these cues triggers cravings and anticipation of the substance’s effects, even if the person is no longer actively using.
- Operant Conditioning: Operant conditioning also reinforces addictive behaviors. In this case, using substances to relieve cravings or negative emotions strengthens the association between the substance and relief. This can create a cycle where people use more to escape negative emotions triggered by the cues.
Examples
- A person who used to smoke cigarettes at a bar might experience cravings when they return to that same bar, even if they haven’t smoked in a long time. (Cue: Bar environment)
- Someone who used cocaine to cope with anxiety might start to crave the drug again when feeling anxious, even in a completely different environment. (Cue: Emotional state)
Importance in Addiction Treatment
Understanding stimulus control is crucial for developing effective addiction treatment programs. Here’s how it’s incorporated:
- Exposure Therapy: This therapy technique involves gradually exposing individuals to drug cues in a safe and controlled setting. They learn coping mechanisms to resist cravings without using the substance.
- Relapse Prevention: Identifying and avoiding high-risk situations or triggers is a critical strategy in relapse prevention.
Cognitive Control of Behavior in Addiction
Cognitive control of behavior refers to the mental processes that enable us to focus our attention, resist impulses, and make deliberate choices. In the context of addiction, cognitive control becomes particularly important because addiction disrupts these very processes. Here’s a closer look at how cognitive control is impaired in addiction and its implications:
How Addiction Weakens Cognitive Control
- Reward System: Addiction hijacks the brain’s reward system, making drug-related cues more salient and cravings more intense. This can make it difficult to resist impulses to use the substance, even when you know it’s harmful.
- Prefrontal Cortex: The prefrontal cortex, a brain region crucial for decision-making and impulse control, is often compromised in addiction. This can lead to difficulty planning, weighing long-term consequences, and resisting urges.
- Decision-Making Biases: People with addiction may be more susceptible to decision-making biases. For example, they might discount the future negative consequences of drug use or overestimate their ability to control themselves.
Consequences of Impaired Cognitive Control
- Increased Vulnerability to Relapse: Difficulty resisting cravings and impulses can significantly increase the risk of relapse, even after a period of abstinence.
- Poor Decision-Making: Impaired cognitive control can lead to poor decisions in various life domains, such as neglecting responsibilities, engaging in risky behaviors, or jeopardizing relationships.
- Mental Health Issues: Difficulties with cognitive control can also contribute to the development or worsening of mental health problems like anxiety or depression, which can further complicate addiction recovery.
Addiction Treatment and Cognitive Control
- Cognitive Behavioral Therapy (CBT): This form of therapy can help individuals identify and challenge unhealthy thoughts and beliefs that contribute to addictive behaviors.
- Attention Training: Exercises designed to improve attention and focus can benefit individuals struggling with impulsivity and difficulty resisting cravings.
- Mindfulness Techniques: Mindfulness practices can help individuals become more aware of their thoughts, feelings, and urges, allowing for more conscious responses instead of impulsive actions.
By addressing cognitive deficits, addiction treatment can empower individuals to regain control of their thoughts, behaviors, and, ultimately, their recovery journey. Overall, cognitive control plays a critical role in addiction and recovery. By understanding the ways addiction disrupts these processes, treatment approaches can be tailored to strengthen cognitive skills and promote long-term success.

Three-Stage Cycle of Addiction
The three-stage cycle of addiction is a widely recognized model that describes the progression of addictive behaviors. It emphasizes the cyclical nature of addiction, where individuals move through stages defined by specific thoughts, emotions, and behaviors. Here’s a breakdown of the three stages:
1. Binge/Intoxication
- Focus: This stage is characterized by the active use of the addictive substance and the experience of its rewarding effects. People may use the substance to cope with negative emotions, enhance pleasure, or relieve stress.
- Key behaviors: Increased drug use, neglect of responsibilities, engaging in risky behaviors to obtain the substance.
- Psychological aspects: Intense cravings, preoccupation with obtaining the substance, euphoria or pleasure during intoxication.
2. Withdrawal/Negative Affect
- Focus: This stage occurs when the effects of the substance wear off, leading to withdrawal symptoms and a range of negative emotions.
- Physical symptoms: These can vary depending on the substance but may include fatigue, nausea, headaches, tremors, or anxiety.
- Psychological aspects: Irritability, depression, anxiety, dysphoria (feeling unwell), shame, and guilt.
3. Preoccupation/Anticipation
- Focus: This stage is characterized by a mental obsession with the substance and a strong desire to use it again.
- Behaviors: Here, the individual plans and strategizes to obtain the substance, their craving triggers become more prominent, and they begin to isolate socially.
- Psychological aspects: Intense cravings, anticipation of relief from withdrawal symptoms, difficulty concentrating on anything else.
Important points to consider:
- Cyclical nature: The three stages form a cycle. The relief from withdrawal symptoms experienced during binge/intoxication can reinforce the desire to use again, leading back to preoccupation/anticipation.
- Individual variations: The experience of each stage can vary depending on the individual, the specific substance, and the severity of addiction.
- Not linear: People with addiction may not always linearly progress through the stages. There can be relapses at any point.
Understanding the three-stage cycle of addiction is valuable. It offers a model for understanding the motivations and behaviors associated with addiction. Also, by understanding the cyclical nature of addiction, treatment approaches can address cravings, withdrawal symptoms, and the underlying triggers that fuel the cycle. Recognizing the signs and symptoms of each stage can help individuals identify triggers and develop coping mechanisms to prevent relapse. The three-stage cycle is a simplified model, but it provides a helpful foundation for understanding the dynamics of addiction and the challenges faced by individuals struggling with it.
What causes addiction in the brain?
Addiction is a complex disease that disrupts the brain’s reward system, motivation, memory, and learning. It can lead to uncontrollable use of substances or behaviors despite adverse consequences.
Wolfram Schultz et al., in their 2000 study titled ‘Dopamine reward prediction error signal in primate dopamine neurons, ’ show that our brains release dopamine when humans engage in pleasurable activities. Dopamine signals to the brain that something good is happening, motivating us to repeat the behavior. Addictive substances and behaviors hijack this reward system, causing the brain to release dopamine in much more significant amounts than usual. This intense pleasure surge creates an influential memory association between the addictive substance or behavior and the feeling of reward.
Over time, the brain adapts to these repeated dopamine surges by reducing its dopamine production and decreasing the number of dopamine receptors. This means that the person needs more and more of the addictive substance or behavior to experience the same level of pleasure. This is what leads to tolerance, a hallmark of addiction.
As the effects of the addictive substance or behavior wear off, the brain goes into a state of withdrawal. This results in several unpleasant symptoms, such as anxiety, restlessness, and irritability. These withdrawal symptoms can be very intense and drive the person to use the substance or engage in the behavior again to relieve the discomfort.
While dopamine plays a central role in addiction, other brain chemicals are also involved. For example, glutamate is involved in learning and memory, and GABA is a calming neurotransmitter. Addictive substances can disrupt the balance of these chemicals, which can contribute to the symptoms of addiction.
The good news is that addiction is a treatable disease. With treatment, people with addiction can learn to manage their cravings and rebuild a healthy life. Treatment may include medication, therapy, and support groups.
What are the most common causes of addiction?
There is no single statistic as to what the most common causes of addiction are. This is because, as the National Institute of Drug Abuse (NIDA) shows, addiction is a complicated puzzle. Many pieces, including cultural norms, social circles, situations, personality, biology, and even beliefs, fit together.
There are so many different theories about addiction because they focus on various pieces of the puzzle. Some theories say genes or brain chemistry play the most significant role, making some things feel more rewarding than others. Others highlight personality traits like impulsivity, a desire for excitement, or mental health issues stemming from past traumas. Still, others focus on how social and economic factors like solid family bonds, good friends, and opportunities for education and work can influence your choices.
Help needed with a Addiction? Come to our Treatment Centers in West Palm Beach Florida, we can help you!
Our addiction treatment centers in West Palm Beach, Florida offer comprehensive programs that address the physical, psychological, and social factors of addiction using the biopsychosocial model, personality theories and neuropsychology.
Our experienced staff and evidence-based treatments can provide the support and resources needed to overcome addiction. Contact us today to learn more about our programs and how we can help you or your loved one on the road to recovery.

Share This Post