Despite a century of scientific and medical progress, addiction remains a perplexing issue. The question of its cause and definition continues to be a source of debate. The psychology behind addiction is a tangled web, encompassing the disease vs. personal failing argument, the influence of lifestyle and childhood experiences, family history, socioeconomic factors, and countless other, often unquantifiable variables.
How can Physiological things cause an Addiction?
A powerful combination of physiological and psychological factors fuels addiction. Physically, addictive substances or activities hijack the brain’s reward system, flooding it with dopamine and creating a solid association with pleasure.
Over time, the brain adapts to this surge by decreasing its dopamine production, leading to tolerance and withdrawal symptoms. This physiological dependence creates a powerful drive to seek out the addictive substance or activity despite adverse consequences.
Furthermore, these physiological changes can be amplified by psychological factors like stress, anxiety, or a history of trauma. These negative emotions can further trigger cravings and make it difficult to resist the urge to use. Understanding this complex interplay between physiological and psychological factors is crucial for developing effective treatment plans to combat addiction.
Psychological Causes of Addiction
Mental Health Disorders
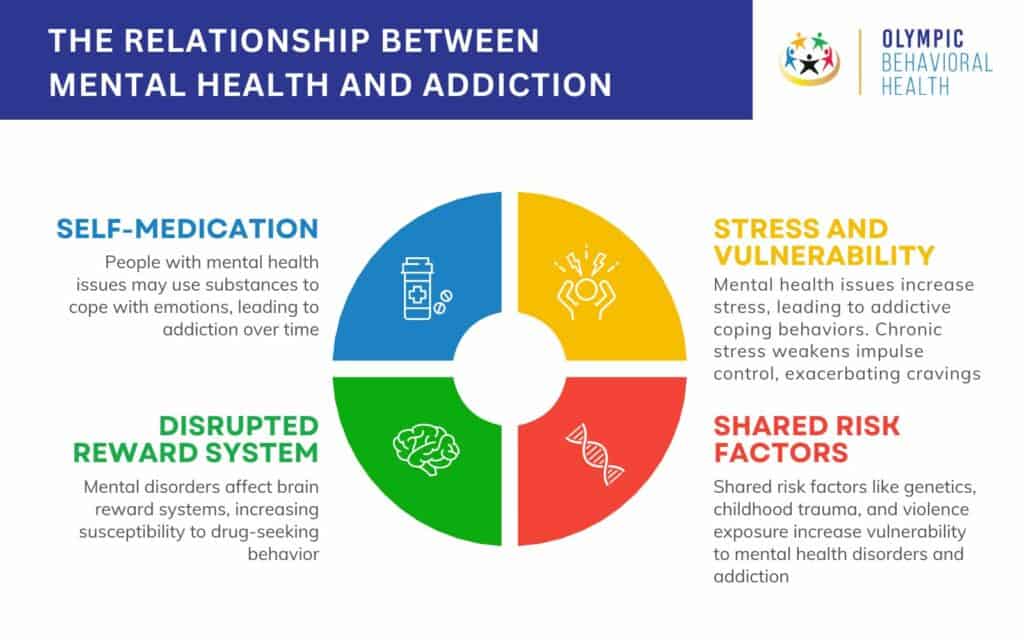
Mental health disorders and addiction often have a complex, intertwined relationship. Mental health disorders are defined by the National Institute of Mental Health (NIMH) as “conditions that affect a person’s thinking, feeling, and behavior.” These can encompass a wide range, including anxiety disorders, depression, bipolar disorder, eating disorders, personality disorders, and schizophrenia.
How Does Mental Health Disorders Cause Addiction?
- Self-Medication: Individuals grappling with mental health disorders may turn to substances like alcohol or drugs to cope with challenging emotions like anxiety, depression, or trauma. These substances can offer temporary relief, creating a belief that they are “necessary” to function. Over time, this reliance can morph into a full-blown addiction.
- Disrupted Reward System: Many mental health disorders impact the brain’s reward system, the same system activated by addictive substances. This can make individuals with these disorders more susceptible to the pleasurable effects of drugs and alcohol, driving them to seek them out repeatedly.
- Stress and Vulnerability: Mental health disorders can be a significant source of stress, making individuals more likely to turn to addictive behaviors as a coping mechanism. Chronic stress can also weaken impulse control, hindering the ability to resist cravings.
- Shared Risk Factors: Some mental health disorders and addiction share common risk factors, such as genetics, childhood trauma, and exposure to violence. These factors can increase vulnerability to both conditions.
Example
Mark experiences chronic anxiety, making daily life a constant struggle. He starts using marijuana to calm his racing thoughts and find temporary relief. Over time, marijuana use becomes a crutch, and its effects on the reward system make him crave it more and more. Mark eventually struggles to function without marijuana despite the negative impact on his work and relationships.
Impulsivity and Risk-Taking Behavior
Impulsivity and risk-taking behavior are significant factors that can increase a person’s susceptibility to addiction. According to the American Psychological Association (APA), impulsivity is “acting without forethought.” It’s the tendency to act on urges or desires in the moment, often without considering the potential consequences. While for risk-taking behavior the National Institute on Drug Abuse (NIDA) defines risk-taking behavior as “actions that increase the chance of harm or negative consequences.” This behavior often involves seeking excitement or thrills, even when danger is present.
How Does Impulsivity and Risk-Taking Behavior Cause Addiction
Here’s how these traits can fuel addiction:
- Difficulty with Delayed Gratification: Individuals with high impulsivity struggle to wait for rewards. They prioritize immediate gratification, leading them to seek out activities that deliver quick pleasure, like substance use or gambling.
- Heightened Sensation-Seeking: People who enjoy risk-taking often crave intense experiences. Addictive substances and activities can provide a robust and immediate source of stimulation, fulfilling this desire.
- Poor Impulse Control: Impulsivity makes it difficult to resist urges and cravings. When faced with temptations, such as drugs or gambling opportunities, individuals might struggle to say no, leading to repeated use and potential addiction.
- Negative Reinforcement: Sometimes, addictive behaviors can provide a sense of relief from negative emotions or boredom. For example, someone might gamble to escape everyday stress, reinforcing the behavior as a coping mechanism.
Example
Mark struggles with impulsivity. He receives a large bonus at work and decides to spend it all at a casino on a single night instead of saving or investing it. The allure of a quick win outweighs the potential for losing everything, demonstrating his difficulty with delayed gratification. This impulsive behavior could lead to significant financial problems and gambling addiction.
Low Self-Esteem
Low self-esteem and addiction are, unfortunately, intertwined. Psychology Today says low self-esteem is “having a negative perception of oneself and one’s abilities.” It involves feeling inadequate, worthless, or unlovable.
How Low Esteem Causes Addiction?
Several mechanisms explain how low self-esteem can lead to addiction:
- Escape from Negative Emotions: People with low self-esteem often experience negative emotions like self-criticism, loneliness, and anxiety. Addictive substances or behaviors can provide a temporary escape from these feelings. For example, alcohol might numb emotional pain, or gambling might offer a fleeting sense of accomplishment.
- Seeking Validation and Worth: Individuals with low self-esteem may crave external validation and a sense of worth. Addictive behaviors can provide a distorted sense of achievement or acceptance. For example, excessive social media use might temporarily boost self-esteem through likes and comments.
- Impaired Decision-Making: Low self-esteem can cloud judgment and make it challenging to make healthy choices. This can lead to poor impulse control and increased vulnerability to the allure of addictive substances or activities.
Example
Mark feels insecure about his appearance and struggles with social anxiety. Mechanism: Seeking Validation and Worth Example: Mark spends hours on social media platforms, constantly seeking validation through likes and comments. He neglects his relationships and responsibilities as he depends on online approval for a sense of worth.
Stress
Stress, a shared experience in modern life, can be a significant trigger for addiction. Let’s delve into the mechanisms behind this connection. According to the American Psychological Association (APA), stress is “the body’s response to a demand.” A variety of events, both positive and negative, can cause it.
How Does Stress Cause Addiction?
Chronic stress can push individuals towards addiction in several ways:
- Hijacked Reward System: When stressed, the body releases stress hormones like cortisol. These hormones can disrupt the brain’s reward system, making people more likely to seek out pleasurable activities or substances to compensate for the negative feelings associated with stress. Drugs and alcohol can artificially activate the reward system, providing temporary relief that reinforces addictive behaviors.
- Increased Cravings: Stress can intensify cravings for addictive substances. This is because the brain associates these substances with relaxation and relief. When stressed, people may crave these substances even more intensely, making it harder to resist them.
- Impaired Impulse Control: Chronic stress can weaken impulse control, making it difficult to resist urges to use addictive substances. This can lead to relapses even after periods of abstinence.
- Self-Medication Attempt: People may turn to addictive substances as a way to cope with the negative emotions associated with stress, such as anxiety, depression, or irritability. These substances can provide a temporary escape, leading individuals to believe they “need” them to manage stress.
Example
John experiences chronic stress and feels overwhelmed. He starts smoking cigarettes to cope with his anxiety and find a sense of calm. Over time, he becomes dependent on nicotine, using cigarettes more frequently to manage his stress despite the adverse health effects.
Personality Disorders
Personality disorders are a group of mental health conditions characterized by inflexible and maladaptive patterns of thinking, feeling, and behaving. These patterns can significantly increase a person’s risk of developing addiction. The American Psychiatric Association (APA) defines personality disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as “enduring patterns of inner experience and behavior that deviate significantly from the expectations of the individual’s culture.” These disorders are typically diagnosed in adulthood and can cause significant distress and impairment in daily life.
How Personality Disorders Cause Addiction?
Several mechanisms connect personality disorders with addiction.
- Emotional Dysregulation: Many personality disorders involve difficulty managing emotions. People with these disorders may turn to substances to cope with intense emotions like anger, anxiety, or emptiness.
- Impulsivity and Risk-Taking Behavior: Some personality disorders, such as borderline personality disorder and antisocial personality disorder, are characterized by impulsivity and a tendency to engage in risky behaviors. This can lead to using substances impulsively or in dangerous situations.
- Poor Coping Mechanisms: Individuals with personality disorders often lack healthy coping mechanisms for dealing with stress, negative emotions, or interpersonal difficulties. Addiction can become a maladaptive coping strategy to manage these challenges.
- Relationship Issues: Personality disorders can make it challenging to maintain healthy relationships. This social isolation and loneliness can lead people to turn to substances for comfort or connection.
Example
Mark struggles with BPD, experiencing intense mood swings and difficulty maintaining stable relationships. He starts using cocaine to manage his emotional highs and lows, initially finding temporary relief. Over time, his cocaine use escalates, causing problems at work and damaging his relationships.
Genetic Predispositions
Addiction is a complex disease with both environmental and genetic components. While the environment plays a significant role, genetic predispositions can make some individuals more vulnerable to developing addictions. Genetic predisposition refers to the increased likelihood of inheriting a particular trait or disease due to specific genes passed down from parents.
How Does Genetic Predisposition Cause Addiction?
Genes don’t directly cause addiction, but they can influence brain chemistry and function in ways that increase vulnerability. Here’s how:
- Neurotransmitter Systems: Genes can influence the production, function, and reuptake of neurotransmitters like dopamine, which play a crucial role in the brain’s reward system. Variations in these genes might make individuals more susceptible to the rewarding effects of addictive substances.
- Stress Response: Some genes are associated with the body’s stress response system. Variations in these genes might make individuals more likely to experience anxiety or depression, potentially leading them to use substances as a way to cope.
- Impulse Control: Genes can also influence impulse control. Individuals with certain genetic variations might be more prone to impulsivity and risky behaviors, making them more likely to misuse substances.
Example
Let’s say Sarah has a genetic variation in a dopamine receptor gene. This variation, as shown by David E. et al. in their 1994 research work ‘The dopamine D2 receptor gene: a genetic risk factor in substance abuse’, might make her less responsive to natural rewards, making her more likely to seek out the intense stimulation of addictive substances to experience pleasure. While this doesn’t guarantee addiction, it does increase her vulnerability compared to someone without this variation.
Important to Note
- Genetic predisposition is not destiny. Environmental factors like childhood trauma, social environment, and access to substances significantly influence addiction risk.
- There’s no single “addiction gene.” Addiction likely results from a complex interaction of multiple genes and environmental factors.
- Genetic testing for addiction risk is still in its early stages and not widely available.
If you’re concerned about your genetic risk for addiction, talking to a healthcare professional can help you understand your situation and develop strategies to mitigate potential risks.
Cognitive Distortions
Cognitive distortions are unhealthy thinking patterns that twist our perception of reality. These distortions can significantly contribute to the development and maintenance of addiction. According to the Beck Institute at the University of Pennsylvania, cognitive distortions are “negative thought patterns that can distort our perceptions of reality.” These patterns can lead to negative emotions and behaviors.
How Cognitive Distortions Cause Addiction?
Cognitive distortions can fuel addiction in several ways:
- Justification and Minimization: People struggling with addiction may use cognitive distortions to justify their behavior. For example, someone might minimize the negative impacts of their substance use by thinking, “Everyone drinks this much” (minimization) or “I deserve a drink after a long day” (justification).
- Negative Self-Beliefs: Cognitive distortions can reinforce negative self-beliefs, leading to feelings of worthlessness and hopelessness. These feelings can then be used as a reason to continue using substances: “I’m a failure anyway, so what does it matter if I use?”
- All-or-nothing thinking: This distortion involves viewing situations in extremes (good or bad, success or failure). Someone with this distortion might use substances after a setback, believing they’ve “blown it all” and need to escape.
- Emotional Reasoning: Believing your emotions are facts can lead to distorted thoughts. For example, someone feeling anxious might think, “I can’t handle this without a drink,” even though it’s not true.
Example
Sarah has been struggling to cut back on drinking. After a stressful day at work, she has a few drinks, intending to stop there. However, she falls into the all-or-nothing thinking trap, believing, “I’ve already messed up, so I might as well keep going.” This leads to her finishing the bottle and further delaying her plans to reduce her alcohol consumption.
Emotional Pain
Emotional pain, a significant and often debilitating human experience, can be a powerful trigger for addiction. Let’s explore how this emotional state fuels addictive behaviors. While there’s no universally accepted definition, emotional pain refers to intense negative emotions such as sadness, grief, loneliness, anxiety, or anger. It can stem from various sources like loss, trauma, abuse, or chronic stress.
How Does Emotional Pain Cause Addiction?
Emotional pain can propel individuals toward addiction through several mechanisms:
- Escape Mechanism: Substances like alcohol or drugs can offer a temporary escape from overwhelming emotional pain. They can numb negative emotions, providing relief, however fleeting. This “escape hatch” can be highly reinforcing, leading to continued use.
- Disrupted Reward System: Chronic emotional pain can disrupt the brain’s reward system, making it less responsive to natural rewards like social interaction or hobbies. Addictive substances can hijack this system, producing artificial feelings of pleasure, which the individual may seek repeatedly.
- Increased Cravings: Emotional pain can trigger intense cravings for addictive substances. The association between the substance and relief from pain can become ingrained, leading to a strong urge to use it whenever emotional distress arises.
- Self-Destructive Behaviors: Feeling overwhelmed by emotional pain, individuals may engage in self-destructive behaviors, including addiction, as a way of coping with or punishing themselves.
Example
Sarah experiences chronic loneliness after losing her spouse. She starts drinking alcohol in the evenings to numb the feelings of isolation and sadness. While alcohol initially provides temporary relief, it ultimately worsens her mood and contributes to social withdrawal, creating a vicious cycle.
Lack of Coping Skills
Life throws challenges our way, and healthy coping mechanisms allow us to navigate them effectively. When these skills are lacking, the risk of addiction rises significantly. The National Institute of Mental Health (NIMH) defines coping skills as “healthy ways to handle stress, adversity, and strong emotions.” These skills help us manage difficult situations without resorting to unhealthy behaviors.
How Does Lack of Coping Skills Cause Addiction?
The lack of coping skills can fuel addiction in several ways:
- Increased Vulnerability to Stress: Life’s inevitable stressors become overwhelming without healthy coping mechanisms. This vulnerability makes individuals more likely to turn to substances as a way to numb or escape difficult emotions.
- Difficulty Managing Cravings: Coping skills can help individuals resist cravings for addictive substances. Without them, cravings become overwhelming, leading to difficulty saying no and an increased risk of relapse.
- Poor Emotional Regulation: Many people use substances to cope with negative emotions like anxiety, depression, or anger. The lack of healthy coping skills makes these emotions even harder to manage, increasing the appeal of substances for temporary relief.
- Social Isolation: Difficulty navigating social situations and relationships can lead to social isolation. This loneliness can then fuel a desire to self-medicate with substances to feel better or connect with others.
Example
Maria has a short temper and struggles to express anger healthily. She starts drinking alcohol to calm down after stressful situations, initially finding it effective. Over time, she develops a dependence on alcohol to manage anger, neglecting her health and relationships due to her drinking.
Trauma
Traumatic experiences can leave deep scars, not just on the mind but also on the brain, increasing the risk of addiction. The National Center for PTSD defines psychological trauma as “a deeply distressing or disturbing experience.” These experiences can overwhelm a person’s ability to cope and can have long-lasting effects on mental and emotional health.
How Can Trauma Cause Addiction?
Several mechanisms explain how trauma can lead to addiction:
- Self-Medication: Trauma survivors often experience intense negative emotions like anxiety, depression, flashbacks, and nightmares. They may turn to substances like alcohol or drugs to numb these emotions and find temporary relief.
- Disrupted Brain Development: Severe trauma, especially in childhood, can disrupt the development of the brain’s reward system, making individuals more susceptible to the rewarding effects of addictive substances.
- Increased Stress and Cravings: Trauma can leave individuals in a chronic state of stress, making them more likely to seek out ways to cope, potentially turning to addictive behaviors. Stress can also intensify cravings for substances that were previously used to manage.
- Avoidance and Emotional Dysregulation: Trauma survivors may develop unhealthy coping mechanisms like avoidance and emotional dysregulation. They might use substances to avoid painful memories or emotions, leading to a cycle of addiction.
Example
Sarah experienced physical abuse as a child. She struggles with anxiety and post-traumatic stress disorder (PTSD), often reliving traumatic memories. She starts drinking heavily to numb her emotional pain and avoid these memories. Over time, alcohol becomes her primary coping mechanism, leading to dependence and addiction.
Fear of Withdrawal
Fear of withdrawal is a powerful force that can trap people in the cycle of addiction. Withdrawal is a set of physical and psychological symptoms that occur when someone dependent on a substance abruptly stops using it. These symptoms can range from mild discomfort to life-threatening, depending on the substance and the severity of dependence.
This fear of withdrawal is the intense anxiety and dread associated with the potential withdrawal symptoms. It can be a significant barrier to quitting substance use.
How Does Fear of Withdrawal Cause Addiction?
Here’s how fear of withdrawal fuels addiction:
- Negative Reinforcement: Withdrawal symptoms are unpleasant. People with addiction learn that using the substance again is the quickest way to relieve these negative feelings. This negative reinforcement strengthens the association between the substance and relief, making it harder to resist use.
- Heightened Anxiety and Stress: The anticipation of withdrawal symptoms can cause significant anxiety and stress. People may use the substance to cope with these negative emotions, creating a vicious cycle.
- Loss of Control Perception: The fear of withdrawal can make people feel like they are not in control of their behavior. This can lead to feelings of hopelessness and a belief that they cannot quit, further fueling addiction.
- Avoidance Behavior: To avoid experiencing withdrawal symptoms, people may continue using the substance even when they want to quit. This reinforces the addictive cycle.
Example
Sarah has been addicted to heroin for several years. She knows that quitting will lead to severe withdrawal symptoms, including nausea, vomiting, and muscle cramps. The intense fear of these symptoms makes it incredibly difficult for her even to consider quitting despite the negative consequences of her addiction.
Belief Systems
Our belief systems, the core set of values and assumptions we hold about ourselves and the world, can play a surprising role in the development of addiction. Belief systems are complex, encompassing our philosophies, values, and expectations about life. Various factors shape them, including cultural background, childhood experiences, and personal interpretations of events.
How Do Belief Systems Cause Addiction?
Several mechanisms explain how belief systems can act as a risk factor for addiction:
- Negative Core Beliefs: People with negative core beliefs about themselves, such as “I’m worthless” or “I’m powerless,” might use substances to escape these feelings of inadequacy or self-loathing. Addiction becomes a way to numb emotional pain and temporarily feel better.
- Quick-Fix Mentality: Beliefs that problems have quick and easy solutions can lead to dependence on substances as a coping mechanism. People with this mindset might turn to drugs or alcohol to avoid dealing with difficult emotions or challenging situations.
- Perfectionism and Performance Anxiety: Some belief systems emphasize perfectionism and achievement. This can create immense pressure and anxiety, leading individuals to self-medicate with substances to cope with performance anxiety or the fear of failure.
- Lack of Self-Compassion: Belief systems lacking self-compassion can make forgiving oneself for past mistakes or setbacks harder. This lack of self-forgiveness can fuel addictive behaviors as a way of self-punishment or escape from guilt.
Example
Sarah grew up in a highly competitive environment where success was heavily emphasized. She developed the core belief that her worth is tied to her achievements. To cope with the pressure and anxiety of maintaining a perfect image, she starts using prescription stimulants to enhance her focus and productivity. Over time, this reliance on stimulants escalates into an addiction, impacting her health and relationships.
Attention-Seeking Behavior
While not a diagnosable mental health disorder itself, attention-seeking behavior can be a symptom of underlying issues and, in some cases, contribute to the development of addiction. There isn’t a universally agreed-upon definition, but psychologists generally describe it as a pattern of behaviors aimed at getting excessive positive or negative attention from others. These behaviors range from mild (exaggerating stories) to more extreme (faking illness or creating dramatic situations).
How Does Attention-Seeking Behavior Cause Addiction?
Here’s how attention-seeking behavior can lead to addiction:
- Validation and Reward: People who rely heavily on external validation for self-worth may turn to addictive behaviors to get the attention they crave. The initial “high” of attention, positive or negative, can be seen as a reward, reinforcing the behavior.
- Social Media Addiction: Social media platforms can become a breeding ground for attention-seeking behavior. The constant pursuit of likes, comments, and followers can become addictive, leading to feelings of inadequacy and a need for more validation.
- Negative Attention Seeking: Some individuals may seek attention through negative behaviors like starting arguments or creating chaos. The drama and intense reactions they evoke can become a form of validation, even if it’s negative.
- Underlying Issues: Attention-seeking behavior can sometimes be a symptom of deeper issues like anxiety, depression, or loneliness. People may use addictive behaviors to cope with these underlying problems and the lack of genuine connection they feel.
Example
Sarah constantly posts on social media, meticulously crafting an image of a perfect life. She thrives on positive comments and feels anxious and depressed when she doesn’t get enough validation. This cycle of needing attention and feeling inadequate drives her to spend excessive time on social media, neglecting her real-life relationships and responsibilities.
Boredom
While not a clinical diagnosis, boredom is a state of feeling unengaged, unfulfilled, and lacking stimulation. Surprisingly, this seemingly benign state can be a significant risk factor for developing addiction. While not a formal disorder, psychologists define boredom as an “unstimulated awareness” characterized by listlessness, apathy, and a lack of interest in one’s surroundings. Boredom can be temporary or chronic, significantly impacting a person’s well-being.
How Can Boredom Cause Addiction?
Several mechanisms explain how boredom can lead to addiction:
- Seeking Stimulation: The brain craves novelty and stimulation. When bored, individuals may turn to addictive substances or behaviors to create excitement and escape the monotony. Substances can provide a quick and intense high, while addictive behaviors offer a temporary escape from the monotony of boredom.
- Dopamine Deprivation: Boredom can be linked to a lack of dopamine, a neurotransmitter associated with motivation, reward, and pleasure. Addictive substances artificially stimulate dopamine release, creating a temporary sense of joy and motivation that is absent during boredom.
- Increased Vulnerability: Boredom can exacerbate existing mental health conditions like anxiety or depression. People struggling with these disorders might be more likely to turn to addictive behaviors as a coping mechanism when feeling bored and lacking motivation.
- Habit Formation: Repeatedly using substances or engaging in addictive behaviors to escape boredom can lead to the formation of solid habits. Over time, these habits become ingrained, making it difficult to resist the urge to engage in them, even if they have negative consequences.
Example
Michael has a monotonous office job and feels unfulfilled in his personal life. He experiences frequent boredom and struggles to find hobbies or activities that engage him. One night, out of boredom, he tries marijuana with a coworker. He enjoys the temporary relaxation and euphoria, starkly contrasting his usual boredom. This experience triggers a cycle of using marijuana to escape.
Grief and Loss
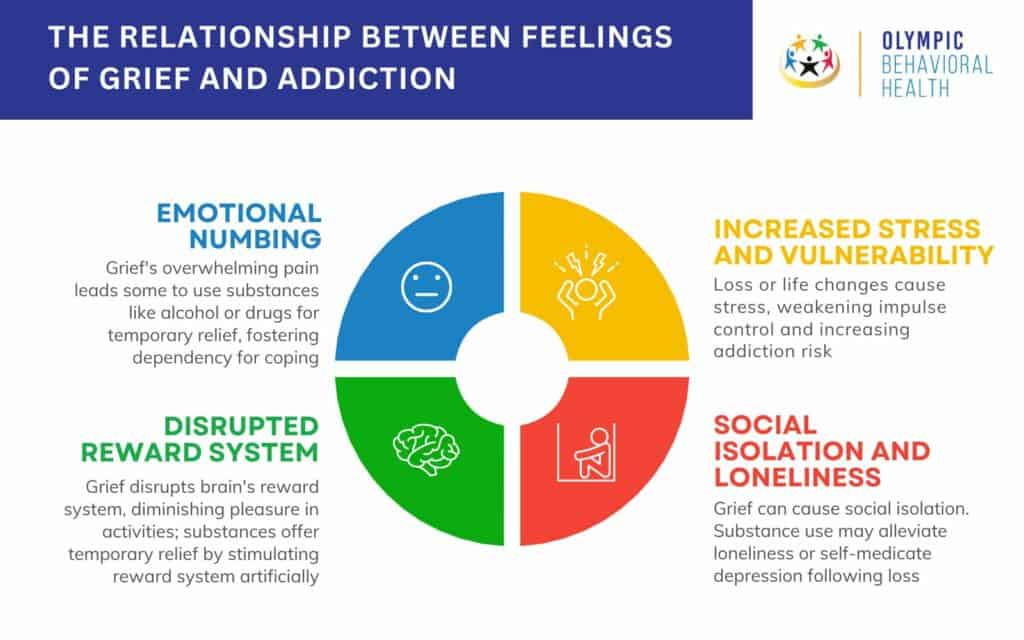
The intense emotional pain of grief and loss can leave individuals vulnerable to addiction. The American Psychological Association (APA) defines grief as “the emotional response to loss.” It’s a natural human experience involving a range of emotions like sadness, anger, guilt, and emptiness.
How Can Grief and Loss Cause Addiction?
Several mechanisms explain how grief and loss can lead to addiction:
- Emotional Numbing: The pain of grief can be overwhelming. People may turn to substances like alcohol or drugs to numb their emotions and escape the emotional turmoil. These substances offer a temporary escape, leading individuals to believe they “need” them to cope.
- Disrupted Reward System: Grief can disrupt the brain’s reward system, making it harder to find pleasure in activities once enjoyed. Substances can artificially stimulate the reward system, providing temporary pleasure and relief.
- Increased Stress and Vulnerability: Losing a loved one or a significant life change is a major stressor. Chronic stress can weaken impulse control and make individuals more likely to turn to addictive behaviors.
- Social Isolation and Loneliness: Grief can lead to social isolation and loneliness. People may use substances to cope with these feelings or to self-medicate for depression that often accompanies loss.
Example
After losing her husband in a car accident, Sarah feels overwhelmed with grief. She starts drinking heavily each night to numb the pain of his absence and avoid confronting her emotions. Over time, she develops an alcohol dependence, neglecting her health and responsibilities to maintain her habit.
Unresolved Anger or Resentment
Unresolved anger and resentment can be a potent cocktail that fuels addiction. Unresolved anger is anger that hasn’t been adequately processed or expressed. It lingers beneath the surface, causing emotional turmoil and impacting behavior. Resentment is defined by the National Alliance on Mental Illness (NAMI) defines resentment as “bitterness or indignation resulting from an injury or insult.” It’s a simmering anger often focused on a specific person or situation.
How Does Unresolved Anger and Resentment Cause Addiction?
Here’s how unresolved anger and resentment can lead to addiction:
- Escape Mechanism: The constant emotional burden of anger and resentment can be overwhelming. Individuals may turn to substances like alcohol or drugs to numb these feelings and find temporary relief.
- Self-Destructive Cycle: Addiction can initially provide a sense of control over negative emotions. However, it worsens the underlying anger and resentment over time, creating a self-destructive cycle.
- Increased Stress: Chronic anger and resentment are significant stressors. This stress can weaken impulse control and increase the desire to use substances.
- Seeking Validation: Unresolved anger can stem from feelings of injustice or wrongness. People may use addictive behaviors like gambling or shopping to feel validated or in control, even if it leads to financial problems.
Example
John was laid off from his job due to an unfair decision by his manager. He feels angry and resentful but avoids confronting the situation. John starts drinking heavily to numb his anger and frustration. While alcohol provides temporary relief, it ultimately damages his relationships and health, worsening his overall situation.
Codependency
Codependency, a relationship pattern characterized by excessive reliance on another person, can create fertile ground for addiction in both the codependent and the person they’re dependent on. The National Library of Medicine defines codependency as “a behavioral pattern characterized by an excessive reliance on a relationship or another person.” People with codependency often prioritize the needs of others above their own, neglecting their well-being in the process.
How Does Codependency Cause Addiction?
Several mechanisms explain how codependency can fuel addiction:
- Enabling Behavior: Codependency often involves enabling the addictive behaviors of others. This might include providing financial support to a struggling addict, making excuses for their behavior, or covering up their mistakes. While done with good intentions, these actions ultimately hinder the addict’s recovery by removing consequences for their actions.
- Loss of Self-Identity: People with codependency often define themselves through their relationships. When their loved one struggles with addiction, their sense of self can be threatened. This can lead to them using substances themself to cope with the stress and anxiety of the situation.
- Low Self-Esteem: Codependency often stems from low self-esteem. Individuals with codependency may believe they are only worthy if they can “fix” or control the person with an addiction. This can lead to feelings of helplessness and hopelessness, potentially turning to substances for emotional escape.
- Stress and Anxiety: Living with a person with an addiction is incredibly stressful. Codependents experience constant worry and anxiety about their loved ones’ well-being. This chronic stress can make them more susceptible to self-medicating with substances to cope.
Example
John struggles with alcoholism. Sarah, out of fear of losing him, constantly covers for his missed workdays due to hangovers or provides him with money for alcohol, believing she’s helping. However, this enables John’s addiction and delays him from facing the consequences necessary to seek help.
Lack of Purpose or Direction
Feeling adrift without a sense of purpose or direction in life can be a significant risk factor for addiction. There’s no official definition, but a lack of purpose is generally understood as a feeling of emptiness, a sense that one’s life lacks meaning or significance. It can manifest as a lack of direction, goals, or a sense of fulfillment.
How Does Lack of Purpose Cause Addiction?
Several mechanisms explain how a lack of purpose can contribute to addiction:
- Existential Void: The absence of purpose can create a deep emptiness and dissatisfaction. This void can drive people to seek temporary fulfillment through addictive substances or behaviors.
- Loss of Motivation: Individuals may need a clear direction or goals to find motivation for healthy activities or pursuits. This lack of motivation can make them more susceptible to the allure of addictive substances or behaviors that offer a temporary escape.
- Low Self-Esteem: Feeling lost and purposeless can contribute to low self-esteem. People struggling with low self-worth may turn to addiction as a way to cope with negative feelings or feel better about themselves, even if only momentarily.
- Increased Stress and Vulnerability: The frustration and uncertainty of not knowing what path to take can be a significant source of stress. This chronic stress can weaken impulse control, making it harder to resist cravings and leading to addictive behaviors as a coping mechanism.
Example
Sarah graduated with a degree but feels stuck in a dead-end job. She experiences a sense of emptiness and purposelessness in her career. To numb these feelings and escape the monotony, she starts abusing prescription pain medication. Over time, her addiction escalates, affecting her work performance and relationships.
Social Anxiety
Social anxiety disorder, a common mental health condition, can create a vicious cycle that leads to addiction. The National Institute of Mental Health (NIMH) defines SAD as “[a]n intense fear of social situations that can cause a person to feel humiliated or scrutinized by others.” This fear can lead to physical symptoms like blushing, sweating, or rapid heart rate, significantly impacting daily life.

How Does Social Anxiety Cause Addiction?
Several mechanisms explain how social anxiety can increase the risk of addiction:
- Self-Medication: People with social anxiety may use substances like alcohol or drugs to “calm their nerves” before or during social situations. These substances can temporarily reduce stress and make social interaction feel easier.
- Negative Reinforcement: The temporary relief provided by substances can reinforce their use. This creates a cycle where social anxiety triggers substance use, which then reduces stress, making it more likely to rely on substances in the future.
- Social Avoidance: Addiction can worsen social anxiety by enabling avoidance of social situations. This can lead to isolation and decreased social skills, further fueling anxiety and dependence on substances.
- Disrupted Reward System: Chronic social anxiety can disrupt the brain’s reward system, making individuals more susceptible to the rewarding effects of addictive substances.
Example
Lisa has social anxiety and experiences extreme fear when giving presentations at work. She starts taking a drink beforehand to calm her nerves and feel more confident. The alcohol initially reduces her anxiety and allows her to perform adequately. Over time, she becomes reliant on alcohol for social situations, neglecting healthier ways to manage her anxiety.
Perfectionism
While sometimes praised for its association with high achievement, perfectionism can have a dark side. It can significantly increase a person’s vulnerability to addiction. There’s no single, universally accepted definition. However, psychologists generally describe it as a personality trait characterized by setting excessively high standards for oneself and others, accompanied by a harsh inner critic and a fear of failure.
How Does Perfectionism Cause Addiction?
Several mechanisms explain how perfectionism can lead to addiction:
- Self-Esteem Tied to Achievement: Perfectionists often link their self-worth to their accomplishments. When they fall short of their unrealistic expectations, they experience intense self-criticism and feelings of worthlessness. This negativity can drive them to use substances to numb the pain or feel better about themselves.
- Chronic Stress and Anxiety: The constant pressure to be perfect creates significant stress and anxiety. People with perfectionism may turn to addictive behaviors like alcohol or drugs to cope with these overwhelming emotions.
- Fear of Failure and Avoidance: The fear of failing to meet their standards can lead perfectionists to avoid challenging situations. This can include avoiding work tasks, social interactions, or creative pursuits. They may then use substances to numb the associated anxiety or boredom.
- All-or-Nothing Thinking: Perfectionists often have an “all-or-nothing” mindset. They may feel like giving up entirely if they can’t achieve perfection. This can lead to using substances to cope with disappointment and feelings of inadequacy.
Example
Emily, a college student, defines her worth based on her grades. She sets unrealistic goals, studies excessively, and avoids social activities. When she receives a lower grade than expected, she feels like a failure and turns to binge drinking to cope with the self-criticism and disappointment.
What are all the potential causes of an addiction?
There are multiple potential causes of addiction, including biological, environmental, and psychological factors. Some people may have a genetic predisposition to addiction, while others may develop it as a coping mechanism for underlying psychological issues such as depression, anxiety, or trauma.
Additionally, environmental factors such as exposure to drugs or alcohol at a young age, peer pressure, and social influence can also contribute to the development of addiction. It is important to note that addiction is a complex issue and may have multiple causes, which is why seeking professional help and support is crucial for recovery.
What are environmental causes of addiction?
Environmental causes of addiction can include a person’s surroundings, upbringing, and social influences. For example, growing up in a household where addiction is prevalent or being exposed to substances at an early age can increase the risk of developing an addiction. Additionally, certain lifestyles or peer pressure can also contribute to addictive behaviors

Share This Post