Fentanyl addiction is a chronic brain disease characterized by an uncontrollable urge to use fentanyl despite its harmful consequences. This powerful synthetic opioid, prescribed for severe pain management, is often misused in illegally manufactured pills or mixed with other drugs, making it highly addictive and potentially lethal.
The physical signs of fentanyl addiction can include nausea, vomiting, blurred vision, constipation, and dizziness. However, the addiction extends beyond physical dependence. Psychological symptoms include intense cravings, anxiety, and depression. Social isolation, neglecting responsibilities, and engaging in risky behavior to obtain the drug are also common signs.
Effective treatment for fentanyl addiction is multi-pronged. Medication-assisted therapy (MAT) uses medications like methadone or buprenorphine to reduce cravings and withdrawal symptoms. Behavioral therapy, such as cognitive-behavioral therapy (CBT), helps individuals identify triggers, develop coping mechanisms, and rebuild a healthy lifestyle. Support groups provide a safe space to share experiences and find encouragement during recovery.
Fentanyl addiction poses a significant risk to a person’s physical and mental health. Long-term use can damage the respiratory system, heart, and reproductive organs. Mental health issues like anxiety and depression are common. The risk of overdose is particularly high due to tolerance, as users may require increasingly larger doses to achieve the same effect.
Preventing fentanyl addiction requires a multi-faceted approach. Public education campaigns should raise awareness about the dangers of fentanyl, particularly its presence in illicit drugs. Harm reduction strategies include distributing naloxone, a medication that reverses opioid overdoses, and providing fentanyl test strips to allow users to check for contamination. Finally, increasing access to effective treatment options like MAT and mental health services is crucial for preventing addiction and promoting recovery.

What is Fentanyl?
Fentanyl is a man-made opioid that’s up to 50 times more potent than heroin and 100 times more potent than morphine. Fentanyl is used as a painkiller for severe pains typically associated with cancer treatment. However, due to its widespread Illicit use, it has some of the highest opioid-related overdose deaths.
Fentanyl works in the parts of the brain that control pain and emotions. There, it binds to opioid receptors. The effects of Fentanyl range from heightened euphoria, dizziness, nausea and vomiting, confusion, constipation, sedation, the development of tolerance, and the potential for addiction, to more long-term effects like respiratory depression and arrest, loss of consciousness, coma, and, severe cases, death.
Can you be Addicted to Fentanyl?
Yes, fentanyl is highly addictive. Fentanyl is a powerful synthetic opioid that is similar to morphine but is 50 to 100 times more potent. It is a prescription drug that is also used illegally. Fentanyl is addictive because it produces feelings of euphoria and pleasure. It also relieves pain. When people use fentanyl repeatedly, their bodies become dependent on it. This means that they need to take the drug to feel normal and to avoid withdrawal symptoms.
A new report by the Substance Abuse and Mental Health Services Administration (SAMHSA) reveals concerning statistics on fentanyl use in the United States. According to the 2022 National Survey on Drug Use and Health, an estimated 991,000 people aged 12 or older misused fentanyl in the past year. This figure breaks down into 686,000 people specifically using illegally made fentanyl (IMF) during that same period.
Fentanyl addiction can be very dangerous. People who are addicted to fentanyl may overdose and die, even if they have used the drug for a short time. This is because fentanyl is so potent, and a small amount can be deadly.
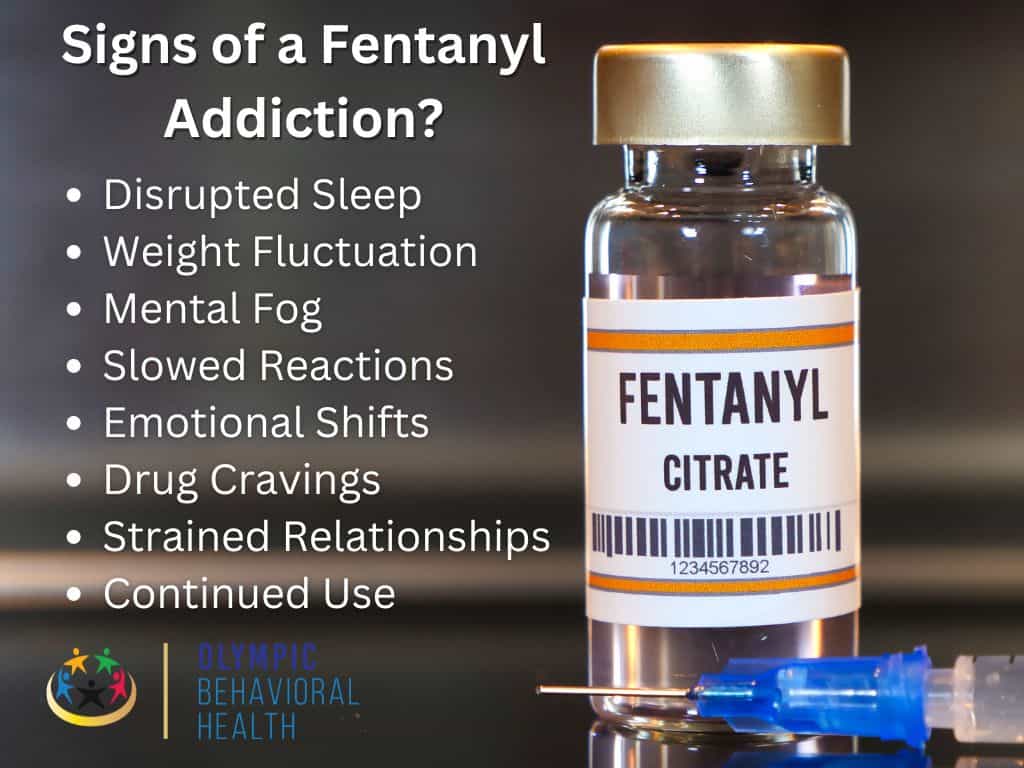
What are the Signs of a Fentanyl Addiction?
Fentanyl, a powerful synthetic opioid, is gripping communities across the country. Its intense effects and prevalence in illicit drugs make addiction a serious threat. But can you recognize the signs? If you suspect someone you know struggles with fentanyl addiction, be aware of these common signs:
- Disrupted Sleep: Significant changes in sleep patterns, including insomnia or excessive sleepiness.
- Weight Fluctuation: Unexpected or sudden weight loss.
- Mental Fog: Difficulty concentrating, focusing, or remembering things.
- Slowed Reactions: Noticeably sluggish reflexes or movements.
- Emotional Shifts: Mood swings, depression, or agitation.
- Drug Cravings: Intense cravings for fentanyl or other opioids.
- Strained Relationships: Problems in personal relationships and social activities.
- Continued Use: Using fentanyl despite negative consequences on health and well-being.
Why is it important to get Treatment for a Fentanyl addiction?
Like any form of addiction, fentanyl addiction has several negative effects on the user. In severe cases, it can result in the death of the user. Here are some reasons why getting treatment for fentanyl addiction is crucial.
- Life-Threatening Overdose: Fentanyl’s potency makes overdose a major risk. Treatment programs can provide education on overdose prevention and access to medications like naloxone that can reverse an overdose.
- Improved Physical Health: Fentanyl addiction can take a toll on the body. Treatment can help individuals regain their health and well-being by addressing the physical effects of addiction.
- Mental and Emotional Wellness: Addiction can cause mood swings, depression, and anxiety. Treatment incorporates therapy to address these underlying mental health issues.
- Stronger Relationships: Addiction strains relationships. Treatment can help people rebuild trust and mend connections with loved ones.
- Sustainable Recovery: Fentanyl cravings are intense. Treatment offers support systems and coping mechanisms to help individuals manage cravings and avoid relapse.
Overall, treatment provides the tools and support needed to overcome addiction and live a healthy, fulfilling life.
What is the Risk of a Fentanyl Addiction?
Fentanyl addiction carries a heavy burden, impacting a person’s physical and mental well-being in numerous ways. Here’s a breakdown of the potential risks:
Short-Term Misery
- Nausea and Vomiting: Fentanyl disrupts the body’s signals for nausea and vomiting, leading to unpleasant experiences.
- Blurred Vision: Constricted pupils caused by fentanyl can make it difficult to see clearly.
- Convulsions: In some cases, fentanyl can paradoxically trigger seizures due to abnormal brain activity.
- Dizziness and Lightheadedness: Fentanyl’s depressant effects can lower blood pressure and reduce blood flow to the brain, causing dizziness and lightheadedness.
- Fatigue: Fentanyl’s sedative properties lead to drowsiness and exhaustion.
- Constipation: Fentanyl slows down bowel movement, making it harder to pass stool.
Long-Term Damage
- Respiratory Problems: Chronic use suppresses breathing, increasing the risk of infections, breathing difficulties, and impaired lung function.
- Reproductive and Hormonal Issues: Fentanyl can disrupt hormone production in both men and women, leading to issues with fertility and birth defects in newborns.
- Physical Dependence: The body adapts to fentanyl’s presence, causing withdrawal symptoms if use is stopped.
- Tolerance: The brain adapts to fentanyl, requiring higher doses to achieve the same effects, increasing the risk of overdose.
- Psychological Dependence: An uncontrollable urge to use fentanyl develops as the brain’s reward system craves its effects.
- Cognitive Impairment: Memory, focus, and decision-making abilities decline with long-term use.
The Downward Spiral
Continued fentanyl use creates a vicious cycle. As the brain adapts, the user experiences both physical and psychological dependence. To overcome tolerance and feel “normal,” they may increase dosage, putting themselves at a higher risk of overdose. Ultimately, addiction takes hold, characterized by a compulsive need for the drug despite its negative consequences.
How Does Someone Get Addicted to Fentanyl?
Fentanyl, a powerful synthetic opioid, is prescribed for severe pain management. However, its potency and accessibility on the illegal market make it highly addictive. But how does someone using fentanyl transition into addiction? Let’s explore the slippery slope that can lead to dependence.
Fentanyl’s allure often lies in its ability to produce an intense euphoric rush. Users may initially seek it out for recreational purposes, unaware of its addictive potential. Prescription misuse can also be a starting point. People taking fentanyl as directed might be tempted to increase their dosage to maintain pain relief, unknowingly crossing the line into dependence.
With repeated use, the body adjusts to fentanyl’s presence. Tolerance develops, meaning higher doses are needed to achieve the same effects. This can quickly escalate use, as individuals chase the initial powerful high.
As tolerance builds, physical dependence sets in. The body starts to rely on fentanyl to function normally, leading to withdrawal symptoms if use is stopped. These symptoms, which can include muscle cramps, nausea, and severe discomfort, become a powerful motivator to continue using, even if the user wants to quit.
Fentanyl’s impact goes beyond the physical. It alters brain chemistry, particularly the reward system. Dopamine, a neurotransmitter associated with pleasure, is heavily influenced by fentanyl. This creates a strong psychological dependence, where the user craves the drug to feel good and avoid withdrawal symptoms.
The combination of physical and psychological dependence creates a powerful cycle. Chasing the initial high, managing tolerance, and avoiding withdrawal all become driving forces in the user’s life. This can lead to neglecting responsibilities, isolating from loved ones, and engaging in risky behavior to obtain the drug.
How can you prevent a Fentanyl Addiction?
Preventing fentanyl addiction requires a multi-pronged approach, focusing on education, harm reduction, and treatment accessibility. Here are some key strategies:
- Education
- Raising Awareness: Increasing public awareness about the dangers of fentanyl, especially its presence in counterfeit pills and illicit drugs, is crucial. Educational campaigns can target teens, young adults, and at-risk populations.
- Prescription Opioid Awareness: Educating healthcare professionals and the public on appropriate prescribing guidelines for pain medication can help prevent misuse and dependence on opioids, potentially leading to fentanyl later.
- Harm Reduction
- Naloxone Distribution: Equipping individuals and communities with naloxone, a medication that reverses opioid overdose, can save lives. Wider accessibility to naloxone empowers people to intervene in case of an overdose.
- Fentanyl Test Strips: Providing access to fentanyl test strips allows people using illicit drugs to check for fentanyl contamination, potentially allowing them to adjust the dosage or avoid using it altogether.
- Treatment Accessibility
- Medication-Assisted Treatment (MAT): Expanding access to MAT programs that combine medication like methadone or buprenorphine with counseling can help individuals struggling with opioid addiction manage withdrawal symptoms and cravings, reducing the risk of relapse and potential fentanyl use.
- Mental Health Support: Addressing underlying mental health issues like depression or anxiety that can contribute to substance abuse is vital. Expanding access to mental health services can promote overall well-being and decrease the risk of addiction.
- Additionally
- Supporting Law Enforcement: Efforts to disrupt the illegal fentanyl trade and hold traffickers accountable can limit the drug’s availability.
- Recovery Programs: Investing in recovery programs that offer comprehensive support, including job training and housing assistance, can help individuals rebuild their lives after overcoming addiction.
By implementing these strategies, we can create a more informed and prepared society, better equipped to prevent fentanyl addiction and its devastating consequences. Remember, addiction is a treatable disease, and with the right support systems in place, recovery is possible.

How Do You Stop a Fentanyl Addiction?
Stopping a fentanyl addiction is a challenging but achievable feat. Here’s a breakdown of the key steps involved:
- Seek Professional Help: Fentanyl withdrawal can be severe and dangerous. Detoxing under medical supervision in a treatment center is highly recommended. Healthcare professionals can manage withdrawal symptoms with medication and monitor your physical health during this critical stage.
- Medication-Assisted Treatment (MAT): MAT programs combine medication with behavioral therapy. Medications like methadone or buprenorphine help reduce cravings and withdrawal symptoms, making abstinence more manageable. These medications are proven effective in managing opioid use disorder and preventing relapse.
- Behavioral Therapy: Therapy plays a crucial role in addressing the underlying causes of addiction and developing coping mechanisms. Cognitive-behavioral therapy (CBT) can help individuals identify triggers, develop relapse-prevention strategies, and learn healthy ways to manage stress and difficult emotions.
- Support Groups: Connecting with others who understand the struggles of addiction can be incredibly valuable. Support groups provide a safe space to share experiences, find encouragement, and build a network of support.
- Address Underlying Issues: Fentanyl addiction often co-occurs with mental health conditions like depression or anxiety. Addressing these underlying issues with therapy can help reduce the risk of relapse and promote overall well-being.
What are the Treatment Options for a Fentanyl Addiction?
Fentanyl addiction poses a serious challenge, but effective treatment options are available. Here’s a breakdown of the main approaches.
Medication-Assisted Treatment (MAT)
Considered the gold standard for treating opioid use disorder, MAT combines medication with behavioral therapy. The medications used in MAT, such as methadone or buprenorphine, work by binding to opioid receptors in the brain, reducing cravings and withdrawal symptoms. This allows individuals to focus on therapy and rebuilding their lives without being consumed by the intense urge to use fentanyl.
Detoxification
The initial stage of treatment often involves medical detoxification. This process helps safely manage withdrawal symptoms under the supervision of healthcare professionals in a treatment center. Medications can be used to ease discomfort, and medical staff can monitor your physical health to ensure a safe and controlled withdrawal.
Behavioral Therapy
Behavioral therapy plays a crucial role in long-term recovery. Techniques like cognitive-behavioral therapy (CBT) equip individuals with the skills to:
- Identify triggers associated with fentanyl use.
- Develop coping mechanisms to resist cravings.
- Address underlying issues that may have contributed to addiction.
- Improve communication and life skills.
Support Groups
Connecting with others who understand the struggles of addiction can be a powerful source of strength. Support groups provide a safe space to share experiences, find encouragement, and build a network of support. These groups can help individuals feel less alone and provide valuable insights from others who have successfully navigated recovery.
Addressing Underlying Issues
Fentanyl addiction often co-occurs with mental health conditions like depression or anxiety. Addressing these underlying issues with therapy is crucial for long-term success. Treating co-occurring disorders can help individuals manage stress and difficult emotions in healthier ways, reducing the risk of relapse.
Additional Considerations
- Tailored Treatment: Treatment plans should be individualized based on the severity of addiction, co-occurring conditions, and the person’s overall needs and circumstances.
- Holistic Approach: Effective treatment addresses the physical, psychological, and social aspects of addiction.
- Long-Term Commitment: Recovery is a process that takes time and ongoing support. Be prepared to commit to treatment for the long haul.
Remember: Don’t hesitate to seek help for yourself or a loved one struggling with fentanyl addiction. With the right support system and a commitment to recovery, a brighter future is possible.
What are the benefits of a Fentanyl Addiction Treatment
Fentanyl addiction can have a devastating impact on a person’s life, but there is hope. Effective treatment offers a multitude of benefits that can help individuals reclaim their health and well-being. Here’s a breakdown of some key advantages:
- Improved Physical Health: Treatment can help manage withdrawal symptoms and stabilize the body’s systems. It can also address health problems caused by fentanyl use, such as respiratory issues or digestive difficulties.
- Reduced Cravings and Relapse Risk: Medication-assisted treatment (MAT) significantly reduces cravings and withdrawal symptoms, making it easier to stay abstinent from fentanyl. Combined with therapy, treatment equips individuals with coping mechanisms to manage triggers and avoid relapse.
- Enhanced Mental Health: Therapy helps address underlying mental health issues that may have contributed to addiction, such as depression or anxiety. By treating co-occurring disorders, individuals learn healthier ways to cope with stress and difficult emotions.
- Improved Relationships: Fentanyl addiction often damages relationships with family and friends. Treatment fosters rebuilding trust and repairing damaged connections.
- Restored Sense of Self: Addiction can lead to a loss of self-esteem and purpose. Treatment empowers individuals to rediscover their strengths and build a fulfilling life.
- Increased Productivity: Recovering from addiction allows individuals to return to work or school with focus and clarity. They can manage their time and responsibilities more effectively.
- Overall Well-being: Treatment promotes a holistic approach to healing, addressing the physical, psychological, and social aspects of addiction. This leads to a significant improvement in one’s overall well-being and quality of life.
Fentanyl addiction can feel like a dead end, but it doesn’t have to be. Recovery through Fentanyl treatment is a real possibility, and some people truly care and want to see you succeed. So I can take the first step towards being healthier, happier person by seeking professional treatment. Consider reaching out to a qualified treatment center like Olympic Behavioral Health for help with your addiction.

Share This Post



